Dry Eye
The most common cause of dry eye is meibomian gland dysfunction
Dry eye disease
Dry eye is a complex disease of the tears and ocular surface and can affect about one in five adults. Dry eye can occur when you don’t produce enough tears to lubricate the eye, or when the tears evaporate too quickly leaving the eye feeling dry.
Dry eye often presents with symptoms including irritation, foreign body sensation, and fluctuating vision. Dryness of the ocular surface is often accompanied with an increase in the saltiness of the tear film which causes corneal inflammation and pain. Dry eye may be related to many factors like your environment, your lifestyle, previous surgery of the eye, and medications taken. However, by far, the most common cause of dry eye, is meibomian gland dysfunction.
Common symptoms of dry eye
- Irritable eyes
- Feeling of something in the eye
- Gritty sensation
- Variable vision when blinking
- Blurred vision when reading or using computer
- Painful, sore eyes
- Redness of the eyes
- Crusting of lashes or lids when waking in morning
- Watery eyes
- Appearance of styes or chalazion
Common causes of dry eyes
- Medications such as antihistamines, antidepressants, oral contraceptives and roaccutane.
- Incomplete blinking
- Sleeping with eyes slightly open
- Dry air and windy environments
- Allergies
- Laser vision surgery
- Cataract surgery
- Meibomian gland dysfunction
Did you know the most common cause of dry eye is meibomian gland dysfunction?
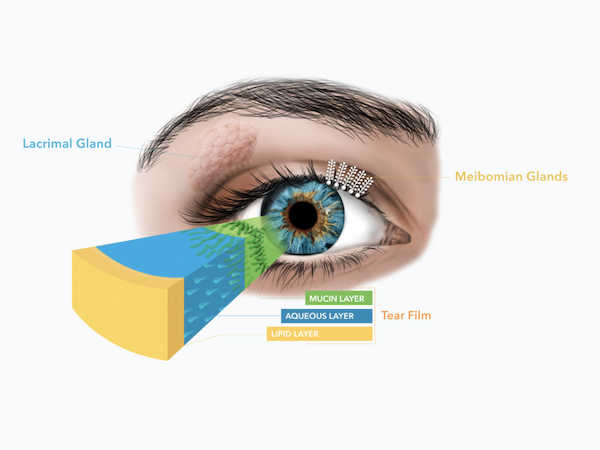
The normal healthy tear layer
A normal healthy tear film is composed of three layers. The inner is the mucin layer which is secreted by goblet cells. The middle layer is the aqueous layer (water layer) which is secreted by the lacrimal gland. Finally the outermost layer is the lipid layer (oily layer) which is secreted by the meibomian glands. Maintaining a perfect balance of these three layers is vital in the prevention of dry eye disease. The most common cause of dry eye is ‘meibomian gland dysfunction’ (MGD) where the meibomian glands fail to produce adequate lipids, causing our tear film to quickly evaporate between blinks.
Meibomian gland dysfunction (MGD)
Meibomian gland dysfunction (MGD) is the most common cause of dry eye disease. Meibomian glands are small vertical oil-producing sacs that reside within the eyelid tissue that have small openings running along the eyelid margin. The role of these natural oils is to coat the surface of our tear fluid and reduce the evaporation of the watery tear fluid layer leaving our eyes feeling smooth and comfortable.
MGD disease refers to inflammation of the meibomian glands within the eyelid margins. When the meibomian glands are inflamed, the amount and quality of oil produced declines leading to burning, itchy, irritated dry eyes. The eyelid margins may also become rough, inflamed and red in appearance. When the tear film does not receive sufficient oil from these glands, the tear layer evaporates at a much faster rate leading to discomfort and damaged cells of the cornea. Prolonged interruption of adequate oil production from these glands may eventually lead to permanent decay of the glands themselves, further intensifying the discomfort of dry eye.
At this practice, we regularly perform meibography which documents the health of your meibomian glands and can be used for future monitoring to ensure no further deterioration of the glands occurs during treatments.

Healthy meibomian glands

Moderate loss of meibomian glands
Potential complications of dry eye
- inflammation and abrasion of the cornea
- ulcers of the cornea
- scarring of the cornea
- loss of vision
- reduce the success of cataract and laser surgery
- cause the slow death of oil producing glands of the eye
- makes contact lens wear uncomfortable
- makes reading books and using computer screens uncomfortable
Our dry eye assessment guide
Questionaire
We use the OSDI questionaire that assesses your dry eye symptoms and the effect it has on your vision. This questionnaire is considered the gold standard for dry eye assessment and can be used for accurate monitoring of dry eye symptoms following dry eye treatment.
Cornea assessment
Various dyes and stains are used with special coloured filters at an illuminated microscope to provide an accurate assessment of corneal tissue health. At a microscopic level it is possible to visualise defects in the corneal epithelium that would not otherwise be observable to the naked eye. These small defects or 'abrasions' contribute to a significant amount of the discomfort associated with dry eye disease. This practice has a microscope that records images of the cornea which can then be compared in the future following dry eye treatments
Tear film analysis
This practice uses sophisticated software combined with Placido disc videokeratography which non-invasively analyses changes in tear film stability. The instrument captures four photokeratoscopic images per second whilst blinking is supressed and this video is analysed to determine the length of time the tear film is stable between each blink. The software automatically saves the information so that future comparisons can be made after dry eye treatment has been commenced.
Meibomian gland assessment
Meibomian glands are meibum or 'lipid' producing glands located in our upper and lower lid margins. The oily meibum produced by these glands coats the surface of the eye preventing the evaporation of the eye's watery or 'aqueous' tear fluid. If meibum quality or quantity is low then the tear fluid on the eye will quickly evaporate leaving the surface of the eye feeling dry. Using an infrared camera, the health of the meibomian glands can be assessed which provides a more accurate management plan for the treatment of dry eye disease.
Lid margin assessment
The eyelid margin is examined using a high powered microscope which can help determine the exact cause of dry eye symptoms. Each eyelid margin contains approximately 25 meibomian glands, each producing 'oil' to protect our tear film from drying out. The general health of these glands and the quantity and consistency of 'oil' is assessed during this examination. Also, the base of the eyelashes is carefully checked for the presence of debris as this directs where attention should be focussed for dry eye treatment.
Tear fluid volume
We carefully evaluate the tear volume using the Schimers test which determines whether the lacrimal gland produces enough tear fluid to keep the eye moist. The Schirmers test is often referred to as the 'dry eye' test. Potential causes of low tear volume include aging, seasonal changes, diabetes, post laser eye surgery, Sjogrens syndrome, systemic conditions such as lupus or rheumatoid arthritis, Vitamin A deficiency, and taking certain medications such as antihistamines and decongestants.
Treatments for dry eye available at this practice
Dry eye disease has many influencing factors, so a treatment plan for one person is likely to be different for another. At Dean Samarkovski Optometrist, we take the time to accurately diagnose the main cause of your dry eye symptoms and then create a treatment plan that not only restore’s comfort to your eyes but also improves the overall health of your eyes. As dry eye disease can be managed, but generally not permanently cured, some form of treatment on an ongoing basis is often to be expected. Ideally, treating dry eye disease ensures no further worsening of the condition, and prevents more long term damage to the delicate glands involved in tear production and the cornea.
Artificial tear supplements
Artificial tear supplements are often the first selected treatment to alleviate the symptoms associated with dry eye. We will recommend a preservative free lubricant drop as preservatives can have a negative impact on the ocular surface of the eye. As dry eye is associated with inflammation of the eye, we may prescribe a short course of steroid eye drops to optimise the comfort of the eyes in the early stages of treatment.

Fortified omega 3 supplements
Research has shown omega 3 supplements may improve the symptoms associated with dry eye and MGD. They work by providing an anti-inflammatory effect which helps reduce the inflammation associated with dry eye disease. The omega 3 also improves the overall tear lipid layer quality, helping to reduce the effects of evaporation from the corneal surface. Not all omega 3 supplements are beneficial. We only recommend high quality omega 3 supplements that have the addition of flaxseed oil and borage oil, which all work together to improve the tear quality and reduce the symptoms associated with dry eye.

Warm compresses
Many people with dry eye find comfort when warm moist heat is applied to their closed lids. Research has shown that around 42 degrees C is an optimal temperature to melt the oil residing in the lipid producing glands of the eye lids (meibomian glands). The softening of the oil allows it to flow freely from the oil glands providing an instant source of lubrication and also preventing evaporation of the aqueous layer of the tear film.

Lid cleansing
Lid hygiene is an important part of a dry eye treatment routine, as it removes unwanted bacteria from our lid margin. An over abundance of normal skin bacteria on the eye lid margin often exacerbates dry eye symptoms. The increased presence of bacteria cause inflammation of the eye lid margins, and contribute to the worsening of the oil quality within our meibomian glands. Regular cleansing of the eye lids and lashes is vital to lessen the impact of dry eye disease and blepharitis. Only particular cleansers are beneficial in dry eye disease as they must contain tea tree oil to be effective.

Punctal plugs
When artificial tear supplements are not enough on their own, a further option is to block the tear drainage duct, preventing your natural tears freely draining away. This can be achieved using punctual plugs which is a reversible procedure performed at this practice. The plugs are made from various materials including soft silicon, a dissolvable synthetic polymer (PCL) and collagen. The silicon plug may last a number of years and can removed at any stage. We commonly use the PCL extended plugs which are effective for 3-6 months after which time they dissolve naturally. These plugs are also great just after eye surgery where the eyes may be temporarily dry, or for dry eye symptoms that are worse at particular seasons of the year.

Blephasteam moisture goggles
Blephasteam is an in-office treatment that we provide for those with mild to moderate MGD. Blephasteam is a medical device that delivers a constant 42 degrees of heat to the eye lids for 10 minutes which is sufficient to melt the obstructed wax like oils with the meibomian glands. The oil secretion is expressed by applying direct pressure to the glands. Typically, this procedure may need to be repeated 3-4 times, once each fortnight to achieve the best results.