Childrens vision
Approximately 1 in 4 children have an undetected vision disorder
Children's eye examinations
Approximately 1 in 4 children have an undetected vision disorder. More than 80 per cent of the information children receive about the world comes through their eyes. Unfortunately, poor vision can effect a child’s development in many ways, including their ability to learn, their coordination, and even personality.
Only a thorough eye examination may detect whether a refractive condition is causing symptoms of blur, eye discomfort or headache. At this practice, children’s eye examinations are conducted with a friendly and caring approach. Dean is renowned for his patience and courtesy when examining children, and having two young daughters of his own, he is very approachable and understanding.
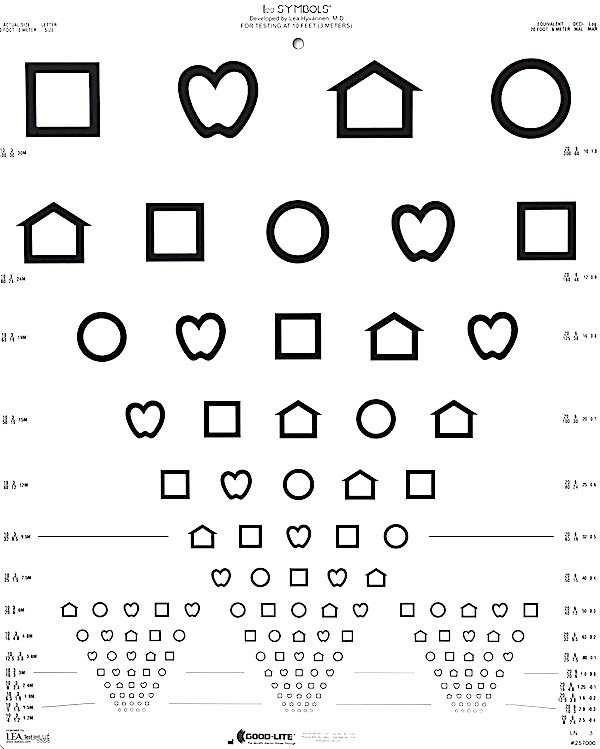
Sharp comfortable vision is paramount for providing the best educational opportunities for children. Unfortunately, most children are not aware of what normal vision looks like and so they do not report any difficulties in their sight until much later after it first begun. The earlier that vision difficulties are detected in children however, the better the potential outcomes of treatment will be.
It is highly recommended that all children should have an eye examination every two years, typically beginning from 3 years of age or 6 months if parents suspect any abnormalities in their childs eyes. Approximately 1 in 4 Australian children have undiagnosed vision disorders which may effect their ability in the classroom. Vision disorders may effect your child’s ability to read a board at school, read books, write, use a computer, and other classroom activities.

Myopia control
Learn more
Ortho-K
Learn more
Common children eye conditions
Myopia, or short-sightedness is a common eye condition that causes blurred vision in the distance. The prevalence of myopia is significantly rising throughout the world, with estimates suggesting by the year 2050, approximately 50% of the worlds population will be myopic.
Risk factors for myopia
Although it is not fully understood why myopia occurs, we do know there are certain risk factors linked to myopia.
- Family history – one myopic parents gives 3x increased risk, and two myopic parents gives a 6x increased risk
- Visual habits – spending greater than 3 hours per day in near activities outside of regular school increases risk by 2-3x
- Lifestyle – spending less than 1.6 hours outdoors every day increases risk 2-3x
Complications of myopia
The presence of moderate to high myopia increases the lifetime risks of sight threatening conditions such as cataract, glaucoma, retinal detachment, and macular degeneration.
How we assess myopia
Myopia is generally confirmed following a thorough eye examination. We measure the vision of your child and the power of the eye (refractive error), the axial length of the eye, and we often using dilating drops to check the internal health of the eye.
Treatment of myopia
In considering treatment options for myopia, we consider the lifestyle of your child, particularly the time your child spends outdoors, and the time spent doing near based activities. Often treatment may include wearing glasses or contact lenses, reducing time spent doing near based activities, increasing time spent outdoors, and compounded weak atropine eye drops. A combination of each of these treatments can be useful for reducing the rate of further myopic progression, and this is often discussed with the parents once myopia has been detected.
Myopia control
Children that develop early onset myopia, have a risk of further progression of their myopia as they develop and undergo growth spurts. Due to the increased eye health risks associated with high myopia, it is recommended that consideration be placed on attempting to slow down the rate of myopic progression in young adolescents (myopia control) . To learn more about myopia control please head to our myopia control information for parents.
Hyperopia, or long-sightedness, is a common eye condition, whereby the eye has to increase its level of focus to maintain clear vision. If the amount of hyperopia is significant enough, then the increased effort required to maintain clear focus may cause eye strain, headaches or even cause the eyes to become crossed inwards. In general, children who have mild hyperopia will not experience problems.
Can I tell if my child has hyperopia?
A complete eye examination is the only sure way of determining whether your child’s vision is normal. Some clues that may suggest your child has hyperopia may include
- headaches during and after near tasks
- one or both eyes appear ‘crossed’ at various times of the day
- tired eyes after prolonged near work
- poor concentration
How we assess hyperopia
Hyperopia is generally confirmed following a thorough eye examination. Most often hyperopic children can see well in the distance, so only measuring the vision of a child will miss the fact the hyperopia is present. This practice will most often use special eye drops that relax the focussing muscles of the child and hence be able to detect all levels of hyperopia accurately.
Treatment of hyperopia
Typically, hyperopia in children is corrected with spectacles, either worn full-time or part-time spending on the level of hyperopia, and whether the eyes are straight in appearance or if one eye is poor in vision. Older children may choose to wear contact lenses as an alternative to glasses.
Astigmatism is a common eye condition where light entering the eye is focussed at two different points either in front of, behind, or partially on the retina. This uneven focussing of light is caused by the curvature of the cornea (front of eye) or lens (within the eye) being ‘football’ or ‘egg’ shaped.
Can I tell if my child has astigmatism?
A complete and thorough eye examination is the only sure way of determine whether your child has astigmatism. Some clues that a child has astigmatism may include;
- ‘squinting’ eyes to see in the distance or up close
- tilting their head to see better
- headaches when reading or watching TV
How we assess astigmatism
Astigmatism is generally confirmed following a thorough eye examination. Most often children with moderate to high levels of astigmatism can not see well in the distance or at near. This practice will most often use special eye drops that relax the focussing muscles of the child and hence be able to detect all levels of astigmatism accurately. It is particularly important to detect moderate amounts of astigmatism in children before the age of 5 so the eyes have a chance to develop normally.
Treatment of astigmatism
Typically, astigmatism in children is corrected with spectacles, either worn full-time or part-time spending on the level of astigmatism, and whether the eyes are straight in appearance or if one eye is poor in vision. Older children may choose to wear contact lenses as an alternative to glasses.
Amblyopia occurs in early childhood when the nerve pathways between the eye and brain are not properly stimulated with clear vision. This visual pathway develops from birth to 8 years of age. If there is some impairment in vision during this critical time, then the vision may remain poor into adulthood. Early detection and treatment of amblyopia is vital. Causes of amblyopia may include:
- a turned eye (strabismus)
- significantly different focussing abilities between the two eyes
- damage to the optic nerve or retina
- cloudy lens of the eye (cataract)
How is amblyopia treated
Amblyopia may be treated successfully in children under 8 years of age. Treatment may include wearing glasses and patching the ‘stronger’ eye forcing the ‘weaker’ eye to work harder allowing critical visual pathways to develop.
How long will my child have an eye patched for?
The frequency and duration of patching is dependent on your child’s vision and age. In general, older children will require longer patching times over a greater period of time, as the effectiveness of patching decreases as a child ages. Also longer treatment times are required for children with poorer vision prior to commencing treatment.
Strabismus is a common condition in children where the eyes do not appear to be aligned or pointing straight ahead. In strabismus (‘turned eye’), when one eye is looking at an object, the other eye may be pointing inwards towards the nose, or outwards towards the ear. Sometimes this misalignment may only occur some times of the day, or else may be present all the time. Also, it is possible the ‘turned’ eye may swap from being the right eye to the left eye and vice versa.
Strabismus and vision
If the eyes are not aligned, the brain receives different information from each eye which can lead to seeing double vision (seeing two objects when there is only one). As this is quite confusing for the brain, children quickly adapt by automatically ‘turning off’ one eye, therefore avoiding the problem if seeing double vision. However, turning off he eye then leads to poor vision in that eye resulting in amblyopia.
Can I tell if my child has strabismus?
Signs of strabismus may sometimes be observed by parents when it is obvious the eyes do not appear straight. In other cases however, the amount the eyes are misaligned may be small or only occur infrequently so can be missed. If your child tends to close one eye, tilts their head to see better, or seem quite clumsy, then it is best to have your child’s eyes examined. Occasionally older children may complain of blurred or double vision or jumping words when reading. As strabismus can occasionally be a sign of a more serious health condition, it is important that children are assessed by an optometrist or ophthalmologist as soon possible when strabismus is first detected.
How we assess for strabismus
We use a variety of tests to determine whether a child’s eyes are straight and working together as a team. At this practice your child will receive eyes drops to dilate the pupils and better control the focussing mechanism of eye so an accurate diagnosis may be made.
Treatment of strabismus
Treatment of strabismus aims to improve the alignment of the eyes and attempt to restore normal vision. Treatment can be varied depending on the cause of strabismus and may include
- full time glasses including bifocals
- eye patching
- surgery to realign the eyes
Blepharitis is a chronic inflammatory condition that typically affects the edges of the eyelids in both eyes. Blepharitis occurs when the tiny oil glands near the base of the eyelashes become congested and blocked. Often this occurs due to an inflammatory response to excessive bacteria along the lid margin.
Symptoms of blepharitis
Symptoms of blepharitis can be varied, but may include
- redness of the eyelids
- crusting on the eyelashes
- burning, stinging eyes
- watery eyes
- sensitivity to light
Treatment of blepharitis
Blepharitis symptoms mostly improve with good eyelid hygiene practices. This may involve daily warm compresses and eyelid cleansing with antibacterial foam cleansers designed to treat blepharitis. However, as blepharitis is chronic, the symptoms may recur if regular eyelid cleansing routines are not maintained.
Should I treat blepharitis?
If blepharitis is left untreated then complications may arise, such as chalazion, conjunctivitis, dry eye disease, destruction of oil glands and lid margin scarring.
Conjunctivitis (‘pink eye’) is the inflammation or infection of the outer membranes surrounding the eye and lining the inner surface of the eye lids. As conjunctivitis can be highly contagious it is important that the causes is accurately determined so appropriate treatment can be commenced.
Symptoms of conjunctivitis
- teary eyes
- puffy eyes and eye lids
- gritty sensation in your eye
- sticky discharge usually worse when waking
- itchy eyes
- sensitivity to light
Causes of conjunctivitis
Conjunctivitis can originate from many sources therefore an accurate diagnosis by an eye health practitioner is important so treatment is commenced early. Causes of conjunctivitis may include;
- bacteria
- viruses
- allergic responses
- irritants
- foreign objects in the eye
- a blocked tear duct
Treatment of conjunctivitis
An accurate diagnosis of the type of conjunctivitis is resent is important for the treatment of conjunctivitis. At this practice we will consider your symptoms and carefully examine the eye with a slit-lamp, taking care to look for damage of the cornea, and presence of foreign material under the eye lids. Treatments may include;
- antibiotic ointment or eye drops
- steroid eye drops
- antihistamine tablets and eye drops
- lubricants
- removal of a foreign object in the eye
Prevention of conjunctivitis
Some forms of conjunctivitis are contagious. Until an accurate diagnosis os made, anyone with conjunctivitis should avoid touching their eyes and also wash their hands regularly. This will reduce the risk of spreading the disease. Also avoid sharing towels, face cloths and ensure children do not attend school until the discharge has stopped in both eyes.