Macular Degeneration
We use advanced technology to assess your eyes
Macular Degeneration
Age-related macular degeneration (AMD) is a common degenerative eye disease effecting 1 in 7 people over the age of 50. As the disease effects the central part of the retina (macula), it causes central vision loss. AMD occurs in two general forms, ‘dry’ and ‘wet’. The dry form results from metabolic breakdown of retinal cells and develops slowly so may go unnoticed. In contrast, the wet form develops quickly causing noticeable distortion of vision. There are a number of effective treatments for wet AMD with early treatment being more successful. Emerging advances in medicine may soon offer similar success in treating the dry form as well, however for the moment, lifestyle modifications are recommended to slow the progression of dry AMD.
'The earlier macular degeneration treatment starts, the more effective it may be, so early diagnosis is essential.'

Normal vision

Early macular degeneration

Advanced macular degeneration
Learn more about the technology in our practice
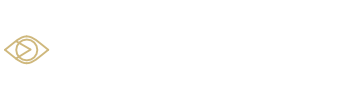
An OCT scan showing early 'dry' AMD (top image) and early 'wet' AMD (bottom image).
Frequently asked questions
Age-related macular generation MD is a degenerative condition that effects the central retina, resulting in a loss of central vision. MD may effect up to one in seven people over the age of 50, and is the most common cause of irreversible vision loss. MD is broadly divided into two types, a dry form and a wet form. The dry form is often slowly in progression and can effect both eyes. It results from central retinal cells slowly losing their function and breaking down. The wet form can be more aggressive in nature and can cause more rapid vision loss. It results from an invasion of abnormal blood vessels underneath the retinal surface leaking and releasing fluid. This fluid loss can occur rapidly and the central vision may suddenly become blurred or distorted
MD is often first detected by an eye care professional during routine examination, however moderate disease may first be noted by an individual due to sudden blurred vision. An eye examination that tests for MD will typically include checking vision and directly viewing the macula using a high powered lens in front of a slit lamp microscope. As early disease may first occur below the surface of the retina, OCT technology has become invaluable in the early diagnosis and ongoing monitoring of macula degeneration.
Depending on whether you have dry AMD or wet AMD, different treatments may be recommended.
For dry MD, although no medical treatment is currently available, lifestyle changes and vitamin supplements may help slow the progression of the disease. Specifically, eating a well balanced diet (eating fish twice a week and leafy greens vegetables daily), exercising regularly, and ceasing smoking are all beneficial. For moderate disease, taking supplements that comply with the AREDS2 study is recommended. Clinical trials evaluating new treatments for dry AMD are ongoing.
For wet AMD, medical treatments are available and although they do not cure the disease itself, the treatments significantly reduce the progression of the disease and may help prevent vision loss. Wet AMD treatment is based on reducing the growth and leakage of blood vessels beneath the retinal surface. These blood vessels are targeted by injecting an anti-VEGF drug into the eye. The frequency and intervals of this treatment is determined by the treating doctor and can be ongoing over a number of years.
Every person has some degree of risk developing AMD however some specific factors can increase your chances further. AMD effects one in seven people over 50. Those with a family history of AMD have a 50% chance of developing the disease. Those that smoke or have previously smoked have a 3x greater chance of developing AMD. Extensive sun (UV) exposure during life may increase your risk of the disease, and finally having high blood pressure and obesity make also increase your risk for developing the disease.
Although you can not alter your age and family history, certain lifestyle changes can reduce your risks and slow down the progression of AMD. Lifestyle choices such as not smoking, exercising regularly, eating a balanced diet (fish twice a week, leafy green vegetables and fruit daily, and a handful of nuts weekly), reducing fats and oils in your diets wearing sunglasses for outdoor activities.
It is recommended an eye test be performed at least annually for those over 50 with a family history of AMD, or those with early signs of the disease, otherwise every two years in all other individuals. It is vitally important that if you do notice any sudden changes in vision, such as blurred vision, and distorted or wavy text, that you consult an eye care professional immediately. This is particularly the case with wet AMD, as the treatment is most effective if treated at the very early stages of the disease. At this practice, we have invested in the latest scanning equipment to help diagnose the earliest possible signs of the disease.