Diabetic Retinopathy
We use advanced technology to assess your eyes
Diabetic retinopathy
Diabetic retinopathy is a condition that causes changes in the retina when someone has diabetes. The disease causes a reduction of oxygen and nutrients being supplied to the retina. When these changes remain undetected, damage of the retinal vessels continue and new ‘leaky’ blood vessels may develop. These new blood vessels leak fluid and cause an accumulation of fluid in the macula or further bleeding within the eye.
'Early diabetic retinopathy causes a minor visual impairment, however it can lead to blindness as the condition worsens'.

Normal vision

Early diabetic retinopathy

Advanced diabetic retinopathy
Learn more about the technology in our practice
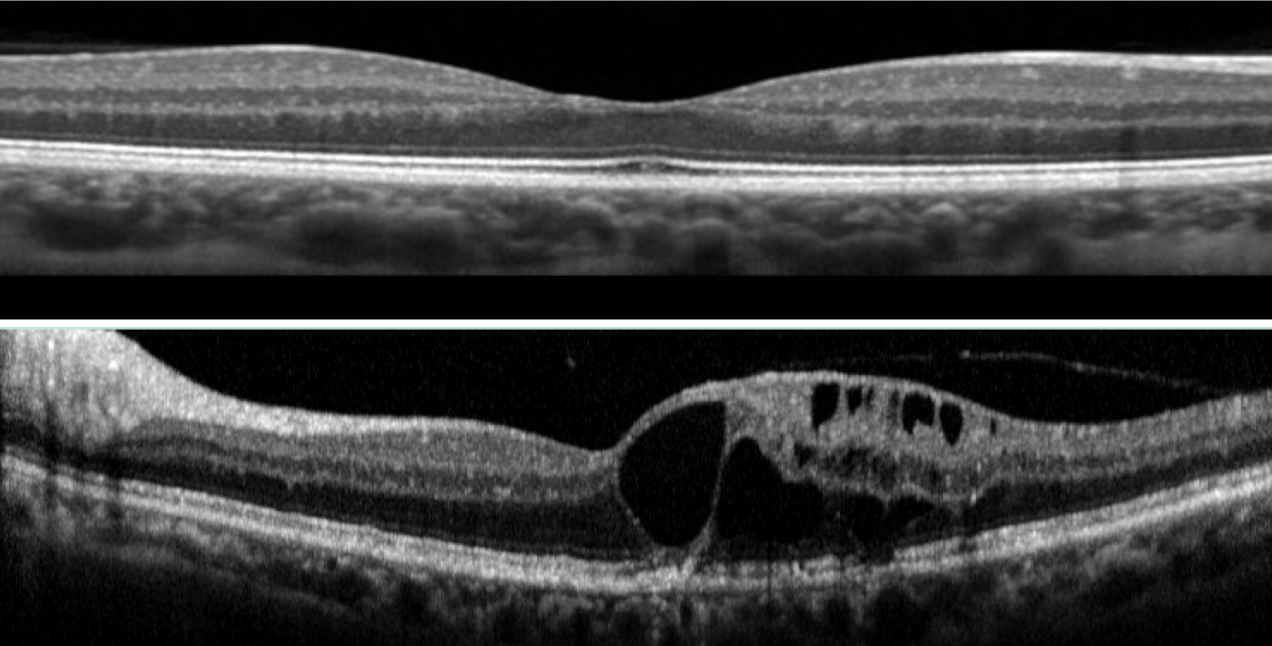
Normal healthy macula scan (top image) compared to diabetic macula oedema (bottom image)
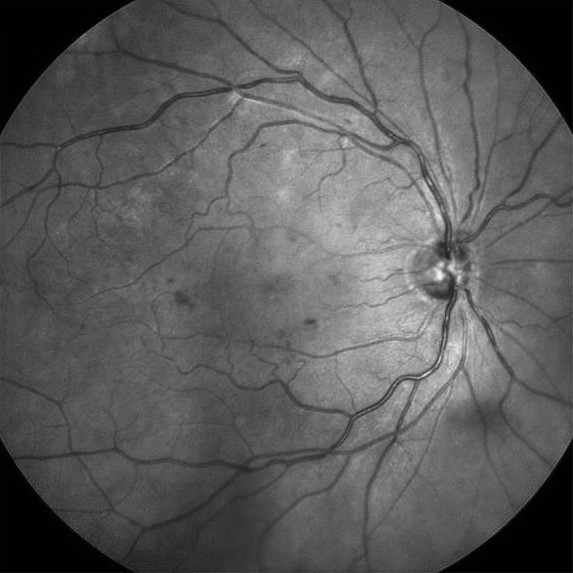
Mild diabetic retinopathy
.
Frequently asked questions
Diabetic retinopathy is a complication that arises in people that have diabetes. These effects are mostly due to the damage of existing blood vessels within the retina, or due to the growth of new abnormally leaky vessels. Diabetic retinopathy can cause significant loss of vision and possible blindness if not treated.
Diabetic retinopathy in the very early stages may not require treatment of the eye itself, however it will require ongoing monitoring of the eye, and improving blood glucose control. However, if diabetic retinopathy progresses to more sight threatening stages, or does in fact cause reduction of vision, then treatments may include a combination of laser therapy, therapeutic injections with the eye and possibly surgery.
Various factors increase the risk of developing diabetic retinopathy. The chance of retinopathy increases with the duration of having been diagnosed with diabetes and certainly increases when blood glucose levels are not maintained at acceptable levels. Indigenous Australians and Middle Eastern groups are up to 4 times more likely to develop diabetes, and well as females that had diabetes during pregnancy. High blood pressure and elevated cholesterol levels increase the risk of diabetic retinopathy, as well as excess weight and smoking.
Lifestyle modifications can significantly reduce the risk of developing diabetic retinopathy. Keeping blood glucose levels in an acceptable range lowers your risk of retinopathy, as does exercising daily, and reducing weight if currently overweight. Ceasing smoking reduces the risk of retinopathy, as does reducing cholesterol to normal levels and reducing systolic blood pressure to 130mmHg or less.
Early stages of diabetic retinopathy usually have no symptoms and can be missed if regular eye examinations are not performed. All people with diabetes should have an eye examination with an optometrist or ophthalmologist every year. Those with additional risk factors such as high blood pressure, obesity, poor glucose control, or early signs of diabetic eye disease may need to be checked more frequently. For those who have been diagnosed as ‘pre-diabetic’ should have an eye examination with an eye care professional at least once every two years.
If any of the following symptoms are noticed, then it is important to have your eyes examined immediately; darks spots in your vision, blurred vision or wavy lines, double vision (seeing two of things), difficulty seeing at night, frequent changes in your spectacle prescription, haloes around lights, and bright flashes of light or dark shadows moving in your vision.